Fatty liver is an extremely common condition that affects 20-30% of all adults. Fatty liver is usually diagnosed on an ultrasound scan of the liver. The liver tests in the blood may or may not be abnormal. Individuals of any age can be affected including young children and adolescents. Most individuals do not have specific symptoms and majority of individuals are often reassured by their doctors of the benign nature of the disease. A certain type of fatty liver is related to excess consumption, but the more common one, which is known as non-alcoholic fatty liver disease or NAFLD affects people who do not drink or drink very little alcohol. Such individuals may have only fatty liver or more commonly suffer from diabetes, high blood pressure, and high cholesterol and triglycerides.
The increasing prevalence of fatty liver is generally linked to overnutrition and sedentary lifestyle. It may be intuitive to believe that a high fat diet can lead to fatty liver; however recent research has highlighted the role of excess carbohydrates in our diet as the cause of fatty liver. Carbohydrates are generally the sweet substances in our diet such as table sugar, fruits, juices, carbonated drinks, candies and related food items. Among the sugars, it is one particular type called fructose that has been found to be most damaging to the liver. Fructose is a simple sugar present in fruits and honey. Table sugar (sucrose) also contain fructose. High fructose corn syrup (HFCS) is a sweetener used in many canned foods. Fructose intake has increased remarkably in the last century and currently it constitutes about 15% of total calorie intake of a typical western diet with higher intakes amongst younger individuals and adolescents.
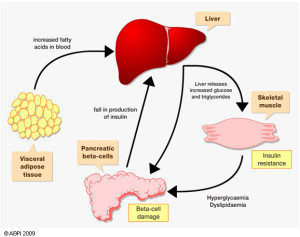
Non-alcoholic fatty liver disease or NAFLD is strongly related to a condition called metabolic syndrome in which affected individuals are overweight and have diabetes or pre-diabetes, high blood pressure, and elevated triglyceride levels in the blood. An affected individual may actually not be quite overweight; instead he or she may just have a large belly or have what is known as abdominal obesity. This form of obesity is extremely common in Asians and Middle Eastern people.
Scientific studies both in animals and humans have shown that a fructose in diet irrespective of other sugars and fats independently is associated with increased fat accumulation in the liver. It has been shown that it takes about 8-24 weeks on a high fructose diet to develop fatty liver. High fructose intake is also associated with development of high blood pressure and elevation of triglycerides in blood, both of which are components of metabolic syndrome. It has even been shown in studies that despite taking a low calorie diet, an individual can still develop fatty liver if the fructose content of diet is high. Another interesting fact is that diabetics who have high blood glucose levels convert the excess glucose to fructose in their liver and this fructose then damages the liver. There are good observational studies that individuals with high intake of sugar sweetened beverage drinks have a higher prevalence of fatty liver. This is alarming because NAFLD is now the most common chronic liver disease in adolescents and this may be related to increased use of sweetened beverages in this age group.
The question that comes up is whether fruits also bad for liver since fruit sugar is actually fructose. Whole fruits are less likely to induce metabolic syndrome because of the lower fructose content per fruit (compared to a soft drink) and because they also contain constituents (flavonols, epicatechin, vitamin C, and other antioxidants) that may combat the effects of fructose.
It has been shown further that a diet rich in fats along with fructose is even more damaging to the liver. Similarly excess glucose intake is also converted in the body to fructose. A high salt diet has also been shown to exacerbate fructose induced liver damage.
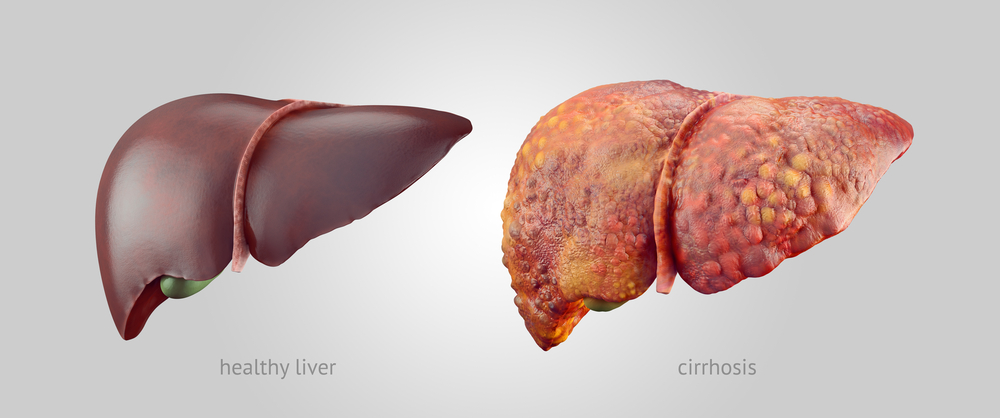
Fatty liver is of two types. The first type is simple fatty liver, also known as NAFL (non-alcoholic fatty liver). NAFL does not usually progress to more advanced forms of liver disease. The second type of fatty liver is known as NASH (non-alcoholic steatohepatitis). NASH is the progressive form of fatty liver and leads to liver fibrosis and eventually to end stage liver disease or cirrhosis. Excess dietary fructose has been associated with NASH. Diabetes is also associated with NASH.
In summary, there has been a marked rise in sugar and high fructose corn syrup (HFCS) intake that has paralleled the rise of fatty liver disease. Experimentally, the fructose component of sugar and HFCS appears to have a major role in inducing fatty liver by both stimulating fat accumulation and inducing liver damage (inflammation). Clinically the intake of sugar sweetened beverages is strongly linked with NAFLD. Reducing sugar or HFCS intake may have major benefits for patients with fatty liver and specially those suffering from the advanced form of fatty liver known as NASH. While whole fruits can be consumed in good proportions, use of sweetened fruit juices, carbonated sweet beverages and food containing HFCS should be curtailed as much as possible. Special emphasis should be given to the fast food diet of children that is rich in fats and sweetened beverages.
Dr. Kaiser Raja (author) is a Senior Consultant in Liver Diseases and Transplantation associated with the Integrated Liver Care Program of the Aster DM Healthcare Group. He is available for consultation in Aster CMI Hospital, Bangalore, Aster Hospital, Mankhool, Dubai and Aster Medical Centre, Hamdan Street, Abu Dhabi.